We Specialise in Contact Lenses!
Here at Mark Hinds Optometrists, we specialise in Contact Lenses. We see many patients with irregular corneas with Keratoconus, corneal grafts and ocular surface disease (etc.) thus needing specialty contact lenses (Please see our page on Specialty Contact Lenses & Ortho-K). But on the other hand, we also have thousands of patients in contact lenses with non-complex eyes, or those who are just sick of wearing glasses.
Dr Mark Hinds is highly trained in the field of contact lenses, so far to the fact that he’s taught and lectured on specialty contact lenses. We use specialty contact lenses every day to help with complex problems only solved with customised solutions.
If you’ve failed at contact lenses before and would like to try again, that is something we’d love to explore and help find a solution. Was it the Comfort? Vision? Conveniences? – These are all things that we can try to work around to find the best solution.
Our contact lens line-up includes:
- Daily
- 2 Weekly
- Monthly
- Toric for astigmatism
- Extended / flexible wear
- Keratoconic / Post Graft / RK / Post LASIK / Extreme Dry Eye / Corneal Hyperalgesia
- Hybrid
- Orthokeratology
- Conventional
- Rigid gas permeable
- Corneo-scleral Contact lenses
- Mini / scleral contact lenses
- Multifocal or bifocal
- Cosmetic / prosthetic
- Tinted
Dr Hinds also has a dedicated clinical trial team. It is common that they are undergoing clinical trials for contact lens manufacturers, in this case some of our patients (who both are willing and fit the criteria) have chance to test new and innovative contact lenses/treatments prior to it being released to the public market. All operations for our patients that participate are overseen by Dr Hinds and have to go through rigorous ethical approval thus you would be in the best standard of care. If you would like to know more or register interest, please visit Ophthalmic Trials Australia.
There are two main types of contact lenses – Soft and Rigid. Soft Lenses are made of a soft gas-permeable water-absorbing material, as silicone hydrogel material that conforms closely to the eye shape. Rigid lenses are usually made of a rigid gas-permeable material and only cover part of the cornea. Mark Hinds Optometrists is only of only few specialty fitters in Australia for the SynergEyes Hybrid contact lenses. These use a silicone hydrogel skirt around a high oxygen RGP centre, meaning that you will get the best of both worlds, a centrally rigid lens and a soft lens exteriorly for enhanced vision and comfort. We have many different designs of this particular lens.
In Australia over 97% of contact lenses prescribed are soft lenses, with the use of rigid lenses generally being reserved for the more specialised forms of contact lens fitting such as:
- High refractive errors,
- keratoconus,
- Corneal ectasia,
- Corneal hyperalgesia,
- Corneal dystrophies,
- Ocular surface disease,
- Orthokeratology &
- Paediatric aphakia
Nearly all the soft lenses prescribed are ‘disposable’ or ‘frequent replacement’ contact lenses, generally designed to be discarded of in a short period of use. This time interval can range from 1 day to 3 months depending on the type of disposable lens.
Contact lenses can be fitted to people of all ages, with our youngest contact lens patient being a baby only a few weeks old, and our oldest contact lens patient (and one of our favourite patients) now 100 years old!
Soft Contact Lenses
- The easiest to wear and get used to.
- Comfortable over longer periods.
- Flexible wearing times.
- Wearer can alter eye colour – from cosmetic to prosthetic.
The most popular mode of lens comprised of differing amounts of water and silicone components, which allows for more oxygen to reach the eye allowing it to ‘breathe more’. There has been a paradigm shift with the latest release of daily disposable contact lenses as more parameters and designs are created. We are early adopters of this new technology and often are getting new lenses 6-12 months prior to market release.
Additionally contact lenses can alter the way your eyes look to others achieved through:
1. Handling Tints
These are simply a light tint to enable the wearer to see them when they drop the lens. This is purely for handling and does not alter the eye colour.
2. Enhancing Tings
Tints are transparent, but add colour to the underlying iris to make the eye more blue, brown, green etc.
3. Cosmetic Tints
These tints enable the wearer to have virtually any colour eye they desire. The colour of the underlying iris is completely blocked out, with the contact superimposing the desired colour on top. Various shapes, colours and logos can all be used.
Hard Contact Lenses
- Lasts longer (needs less replacement).
- More stable for astigmatism.
- Correct vision for: keratoconus, after corneal graft surgery and irregular corneas.
- Costs less over time.
- More dependent upon cleaning and conditioning solutions.
Hard contact lenses or Rigid Gas Permeable (RGP) lenses are a sophisticated option for vision correction. These offer superior clarity and long-term value. These lenses are designed to maintain their shape throughout the day to deliver sharper and clearer vision (Even during blinks). Hard contact lenses do require maintenance; proper cleaning and conditioning is required to maintain the contact lenses lifespan.
Hybrid Contact Lenses
The very latest in design means this material will breathe on the eye, even when you are asleep.
No more coming home late and fumbling around in the dark trying to get your lenses in a case!
Up to 30 days continuous wear is possible with these lenses. Although not suitable for some, they are now proving very popular with the over 40’s who want a break from their glasses.
Contact Lenses can even alter the way your eyes look to others, by changing your eye colour.
This can be achieved by any of 3 means:
1. Handling Tints
These are simply a light tint to enable the wearer to see them when they drop the lens. This is purely for handling and does not alter the eye colour.
2. Enhancing Tints
Tints are transparent, but add colour to the underlying iris to make the eye more blue, brown, green or whatever.
3. Cosmetic Tints
These tints enable the wearer to have virtually any colour eye they desire. The colour of the underlying iris is completely blocked out, with the contact superimposing the desired colour on top. Various shapes, colours and logos can all be used (these are like the ones used in the movies for dramatic effect).
Hybrid Contact Lenses
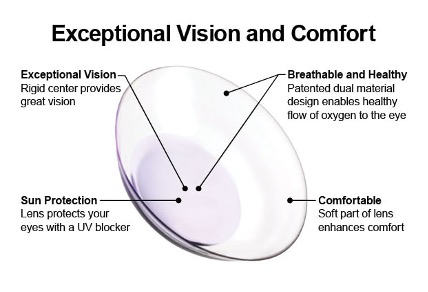
A combination of a silicone hydrogel skirt and a rigid gas permeable contact lens in the centre. The hybrid is the perfect marriage between crisp vision, for those with challenging topography and refractions, and comfort. With this technology at hand, keratoconus is often treated early. We have 100’s of successful and happy patients in these lenses, this being the case we do many of these contact lenses every week and have great success with them. Our most commonly sold at our practice is the Duette UltraHealth contact lenses.
Keratoconus
Keratoconus is presented as a progressive, non-inflammatory thinning and protrusion of the central cornea usually manifesting itself in youth or adolescence however, the age of onset can be anywhere between 7 and 50. Considerable visual impairment can result due to the development of a high degree of irregularity associated with this from surface (‘window’) of the eye. Due to this marked distortion and irregularity, the improvement in vision obtained through spectacles may be minimal. This is where the rigid contact lenses (or similar) come in. Rigid contact lenses are fitted, and they are often the only adequate means of correction for patients suffering from keratoconus. Keratoconus does not cause blindness, but we often bring visual acuity up from counting fingers to near 20/20 vision with our specialty contact lenses.
While the exact cause of Keratoconus remains unknown, there are a few known factors that may cause this disease. Keratoconus can be contracted through both genetic and environmental conditions. Genetically, keratoconus occurs in about 1 in 1,000 to 1 in 4,000 people, in equal frequency in males and females. The hereditary nature however is quite weak, only 10% of people with keratoconus will have an affected relative. Keratoconus is sometimes associated with other conditions such as allergies, asthma, eczema and double jointedness (Margan Syndrome). Environmental conditions such as vigorous eye rubbing eye rubbing or atopic diseases such as hay fever that cause excessive eye rubbing are known causes for keratoconus.
Signs and symptoms of keratoconus include:
- A blurring and distortion of vision that cannot be totally alleviated by spectacle correction.
- Frequent changes in spectacle prescription over a relatively short period of time.
- Reduced vision at night, with ghosting and haloes noticed around lights.
- Multiple images observed (with only one eye).
- Eye strain.
- Headaches.
Progression of keratoconus is quite variable; however, the condition does tend to progress more rapidly the earlier the age of onset. Keratoconus is basically a bilateral condition however, the degree of progression for the two eyes is often unequal and it is quite common for the keratoconus to be far more advanced in one eye. In about 85% of cases, the condition usually stabilizes anytime between 5-15 years after onset. For the remaining 15%, keratoconus progresses to the point where contact lens fitting is no longer possible, where the only treatment is a corneal transplant. Thankfully, corneal collagen cross-linking treatment (CXL) is a great intervention and we have the leading anterior segment ophthalmologists in the world here in Brisbane.
CXL is a non-invasive procedure that is aimed at halting the progression of keratoconus. CXL works by increasing the collagen cross-linking, which helps to prevent the cornea from becoming more conical and irregular, as it would normally with progression of keratoconic condition. During the treatment, riboflavin eye drops are applied to the cornea and then activated by UVA radiation. This process has been shown in laboratory and clinical studies to increase the amount of collagen cross-linking in the cornea, thereby resulting in a stronger cornea. We now have hundreds of patients post CXL, all of which had a positive procedure. We now see treatments with epithelium on and off depending on corneal thickness and the nature of the disease. The latest generation can even give just refractive changes to normal corneas. CXL was first developed in Germany about circa 2000 and has also been refined since 2008 to be a more accurate and quicker process.
In the earliest stages of keratoconus, a spectacle correction may be used to correct the myopia and astigmatism associated with this condition. Soft contact lenses can often also be prescribed during this time for general, recreational or sporting use. As keratoconus progresses, the additional corneal thinning results in the shape of the cornea becoming more irregular to the point that it is not possible to obtain adequate vision with spectacles. At this stage, rigid contact lenses are then required to provide optimal vision. The contact lenses essentially provide a new, regular front surface for the eye, eliminating the distortions caused by the keratoconus. It should be emphasized that, while contact lenses will generally provide a significant improvement in vision, wearing them is not a cure for keratoconus.
The majority of individuals with keratoconus comfortable wear rigid contact lenses throughout the day, enjoying a significant visual improvement. About 10% are unable to tolerate wearing rigid contact lenses due to extreme ocular sensitivity. For this group there are other contact lens options available most notable hybrid contact lenses. Hybrid contact lenses are a good option for keratoconus who play contact sports, as rigid lenses may be easily dislodged during these types of activities.
Keratoconus is a progressive condition; hence it is important that people with keratoconus have regular examinations to monitor the status of their condition and ensure that their contact lenses are still an optimal fit. Poorly fitting contact lenses won’t only just cause increased discomfort (more than that of typical discomfort of a new lens), but it may also worsen keratoconus, this may be due to participants wearing older contact lenses or poorly made/mapped contact lenses. Flat-fitting lenses can lead to corneal abrasions and subsequent corneal scarring; the corneal scarring may then result in a significant reduction in vision.
Only in about 15% of cases of keratoconus does a corneal transplant (graft) become necessary. A corneal graft (or Keratoplasty) is an operation in which the affected (thinned) area of the cornea is removed and replaced by normal tissue, transplanted from a donor cornea. Corneal grafting is required when either a satisfactory fit or normal visual acuity cannot be achieved with contact lenses (this type of scenario is quite uncommon in clinical practice). The success rate for corneal grafts for keratoconus is very high (between 95-100%), although about 60% of people will be required to wear spectacles after a graft and approximately 30% of people will need to wear contact lenses to achieve “normal vision” subsequent to having a graft. Keratoconus, generally, does not reoccur after a corneal graft. There have been a few isolated examples in the past 30 years where this has happened. In these rare cases it is thought that the donor material had inadvertently came from a donor cornea where their descendants had keratoconus.
Orthokeratology
Orthokeratology, also known as Corneal Reshaping Therapy or Ortho-K, is the use of rigid contact lenses to remould the shape of the cornea to reduce or eliminate myopic (Short-Sighted) and astigmatic (irregular surface) errors in the eye. At Mark Hinds Optometrists we have been performing Ortho-K since 2003 and have many patients now living life with clear vision.
Why have Ortho-K done?
The main purpose of Ortho-K is to be rid of both contact lenses and spectacles for the majority of (possible all) waking hours. However, most of our patients in Ortho-K are doing this for the purpose of myopia control.
Is everyone suitable for Ortho-K?
No. At present, Ortho-K is only suitable for shortsighted errors of up to 4.00 dioptres and up to 1.50 dioptres of astigmatism. We have some patients with -7.00D of myopia correction wearing Ortho-K’s, but these patients are the exception not the rule. It is important to note that the Ortho-K procedure is reversible, and we are very conservative treatment wise.
What does Ortho-K involve?
A series of Ortho-K contact lenses made from a highly permeable rigid material are fitted in progressive stages to gently reshape the cornea towards less curvature and a more spherical shape. This reduces near sightedness (myopia) and astigmatism whilst dramatically improvise unaided eyesight. These lenses are generally worn overnight. The full program is often flexible, and higher prescription may require up to ten visits over a six-month period. That being said, generally 4 or 5 visits are expected.
Fees for Ortho-K
The cost for Ortho-K is dependent on the complexity of the prescription. A full price guide will be available once this is established. Your private health fund (where applicable) will be allocated funds for the contact lenses involved in this procedure and a lifestyle bonus may also be applied if available. A full fee disclosure is available at time of consultation, and we ALWAYS perform an initial evaluation and consultation for determination of suitability. We are happy to accept a referral (although not necessary) from your optometrist or ophthalmologist and will give them a comprehensive report if/when required.
Ongoing costs
During the Ortho-K program, each trial lens must be returned at the end of its intended period of use. Lenses not returned or lost or broken will be charged separately. Some lens costs may be claimable from your private health fund. Once the Ortho-K program is complete, you will need to purchase a pair of retainer lenses which is a part of the full fee. The ongoing costs associated with these lenses are usually much less when compared to conventional contact lens wear. The lenses will bast between 2-5 years depending on if your ocular prescription changes (if so, a new pair will be needed), how well the lenses maintain their shape, and how well they are looked after.
So how does it work again?
Similar in appearance to standard contact lenses, Ortho-K therapeutic lenses gently reshape the corneal surface of the eye while you sleep to provide clear, natural vision when the lenses are removed upon waking.
The result is temporary correction of myopia (Short-sightedness) with or without moderate astigmatism (irregular corneal surface). For some people, Orthokeratology slows down or even stops the progression of myopia. Myopia is one of our goals as a (optometric/ophthalmic) society and is gaining in momentum.
What are the benefits of Orthokeratology?
Ortho-K offers freedom from glasses and the hassle of wearing contact lenses during the day enhancing the lifestyle of those requiring vision correction.
Active individuals can freely participate in sports without the interference of glasses or bother of contact lenses during the day. As these special lenses are worn whilst sleeping, eye irritation and dryness often associated with the combination of contact lens wear, extended computer use, and outside dust/pollutants is eliminated. These lenses are very popular with young sports people, people with mild dry eye and those who struggle with contact lenses during the day. Ortho-K is also a great alternative to refractive or LASIK surgery.
Orthokeratology is a safe and effective, surgery free method or managing myopia and low to moderate astigmatism.
Why have I not heard about Ortho-K before?
Orthokeratology has been around for decades, however the recent advances in contact lens technology has brought it to the forefront of myopia control.
The practice of Ortho-K requires a great deal of technical skill and specialised equipment. Mark Hinds Optometrists specialises in contact lens fittings and Orthokeratology, and we are proud to say that we have achieved excellent results amongst our contact lens patient base. This success is specifically found in our management of myopia and low to moderate astigmatism. It is a brilliant result when we can see no change in the short-sighted prescription with kids who, prior, were destined to have “coke bottled glasses”.
If you would like to find out more about Orthokeratology treatment please call us at 07-33586566 to make an appointment or send an enquiry to orders@markhindsoptometrists.com.au.
(Additionally for further research please see www.oso.net.au)
Children and Contact Lenses
The visual benefits that children receive with refractive errors derived from contact lenses are the same as for adults. Children can be prescribed contact lenses for the correction of refractive errors such as myopia, hyperopia and astigmatism. Ortho-K can also be performed successfully on myopia children, although this requires a high level of hygiene, care and compliance. Children who want to wear contact lenses as a preference, sport or cosmetic reason/s can usually be examined, counselled and fitted like an adult albeit with parental guidance at about 8 or 9 years of age. For little ones who have a hyperopic accommodative esotropia contact lenses can straighten up the eyes just the same as spectacles – without the massively positively powered (thick) lenses!
A recent study from the USA indicates that contact lenses can significantly improve social and personal growth. This study focused on how children feel about their appearance and participation in activities in contact lenses compared to spectacles. 71.2% of the children stated that they preferred wearing contact lenses for day to day. 95.9% said they preferred wearing contact lenses during sports, additionally almost 60% of children felt their sporting performance was better while wearing contact lenses. The study went on to conclude that children derive a number of benefits from contact lenses which leads to greater satisfaction with their vision correction.
Children under the age of 7 (including infants and babies) are generally only fitted with contact lenses if there is a specific indication. The most common reason for paediatric contact lens fitting is unilateral or bilateral aphakia (the absence of the natural lens in the eye). Surgical removal of the crystalline lens results in aphakia, commonly due to required cataract surgery. Patients with aphakia will have an extremely high degree of hyperopia (long-sightedness). Contact lenses are definitely the preferred option for the management of aphakia, as aphakic spectacle lenses are incredibly thick (therefore heavy/uncomfortable, especially for children) thus difficult for a baby or young infant to wear. Infants born with congenital cataracts should have them surgically removed as soon as possible (preferably before 3 months of age) with contact lenses being fitted about one week post-operatively. Rigid gas permeable contact lenses are usually the best option for the contact lens management of the paediatric aphake.
Other indications for paediatric contact lens fitting include:
- high myopia and high hyperopia (the latter without aphakia)
- Unilateral ametropia (where the baby/young infant has a significant refractive error only in one eye)
- Corneal Irregularity (usually as a result of trauma)
If you would like to know more about how we perform optometry for young ones, please see our section Children’s Optometry.